Skin tone impacts photoacoustic measurements of blood oxygenation
01 Mar 2022
Pulse oximeters, which measure the percentage of oxygen in the blood, can be used as part of clinical decision-making to triage patients, adjust supplemental oxygen levels, and more. In 2020, researchers analysed tens of thousands of blood oxygenation measurements collected from thousands of patients. The study, though not received without controversy and discussions about study design, found that Black patients had approximately three times the frequency of hypoxemia – an abnormal decrease in the amount of oxygen in the blood – as white patients, and that this condition wasn’t being detected by pulse oximetry in many Black patients. In a letter to the editor in The New England Journal of Medicine, the researchers said that missed hypoxemia diagnoses could result in poorer health outcomes in Black patients.
The NEJM letter grabbed the interest of UC San Diego researchers Jesse Jokerst and Yash Mantri. Jokerst, a professor of nanoengineering, materials science and radiology, and Mantri, a bioengineering graduate student, are working to improve human health using a hybrid light and acoustic imaging technique called photoacoustic (PA) imaging. Soon after the NEJM letter was published, they decided to investigate the impact of skin tone on blood oxygenation measurements obtained using a different tool, PA oximetry.
“[This study] ties into some of our other work in wound imaging, wound repair and regeneration,” Jokerst says. “As we were doing those studies, we became more interested about the impact of skin tone. We also were motivated by the paper in The New England Journal of Medicine, among others, which referenced the impact of melanin in pulse oximetry.”
While pulse oximetry offers a quick and non-invasive way to measure oxygen saturation, pulse oximeters may not account for some physically relevant factors, such as absorption and scatter of photons by melanin in the skin.
And though biomedical optics devices such as pulse oximeters, cerebral tissue oximeters, wearables such as smart watches and PA imagers play “an increasingly powerful role in human health,” Jokerst and Mantri say that few of these devices account for differences in skin tone between individuals. Their subsequent proof-of-concept study, published in Biomedical Optics Express, suggests that individuals with darker skin tones have lower oxygen saturation as determined by PA oximetry compared with individuals with lighter skin tones.
Measuring blood oxygenation with PA oximetry: the physics
Most of the light that hits your skin is absorbed by haemoglobin and melanosomes. Haemoglobin is a protein found in red blood cells that carries oxygen throughout your body. Melanosomes are subcellular organelles that produce and store melanin, which largely governs skin tone – individuals with higher concentrations of melanin have darker skin. Darker skin tones absorb more photons than lighter skin tones because they contain higher concentrations of melanin.
PA oximetry is based on the absorption of light and the thermal expansion of absorbed light in tissue. When visible and near-infrared light from a laser or similar light source is delivered to tissue, it interacts with absorbers such as melanin and haemoglobin in the skin. This absorption of light produces a small temperature increase in tissue that leads to an initial pressure increase and then relaxation.
When the tissue relaxes, acoustic (sound) waves are emitted. The acoustic waves travel to the body’s surface, where they are detected by a PA transducer. The PA signals are used to create images that show the differences in optical absorption in tissue, a source of image contrast that can be used to create maps of oxygen saturation.
Skin tone and PA imaging: proof-of-concept study
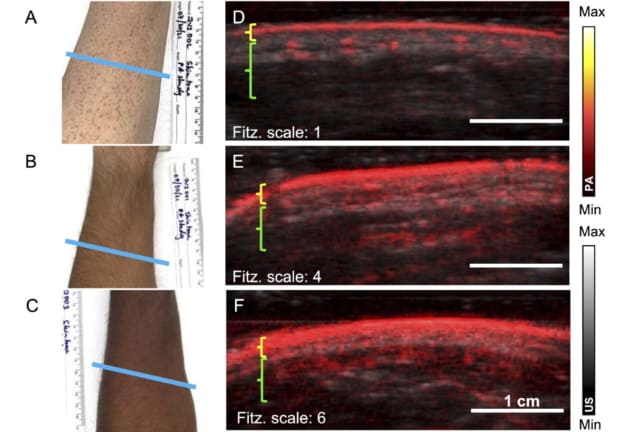
The researchers measured PA signal, penetration depth and oxygenation differences in nine healthy volunteers with three different skin tones. Skin tones were estimated using the Fitzpatrick scale, which is often used in dermatology to estimate the response of different skin tones to ultraviolet light.
Each volunteer’s left arm and hand were imaged in five easily identifiable locations – selected for their relatively uniform distribution of melanin, flat curvature to facilitate scanning and relative hairlessness – using two PA imaging systems. The researchers acquired images using standardized settings that didn’t attempt to compensate for differences in skin tone, and they quantified oxygen saturation using the PA imaging systems’ built-in methods. They also acquired data using a multi-wavelength approach.
Jokerst and Mantri observed that individuals with darker skin tones had higher PA signal intensity at the surface of the skin, with increased acoustic clutter, a phenomenon caused by reverberations or off-axis scatterers. Further studies showed decreased oxygen saturation in the radial arteries of individuals with darker skin tones compared with those with lighter skin tones.
Correcting biases before devices hit the market
For devices on the market, several techniques that try to compensate for measurement biases already exist. PA intensity can be enhanced during image acquisition by adjusting time gain compensation settings. Noise reduction algorithms can also be implemented. Filtered back projection or PA computed tomography could reduce streaking artefacts even when strong absorbers are present. Applying fluence corrections, multi-angle plane wave ultrasound, focused ultrasound, spatial weighting or deep learning could reduce noise and stationary signals that lower the signal-to-noise ratio and mask blood vessels.
Jokerst and Mantri even developed a basic correction factor to adjust PA oximetry measurements. The factor, defined as the ratio between measurements made with these two methods, corrected PA oximetry measurements to within 2% of pulse oximetry.READ MORE

But Jokerst hopes that their study, rather than creating more band-aid solutions, prompts the medical devices community to design devices that account for physically relevant factors such as skin tone before biomedical optics devices go to market. (The first PA imaging device approved by the US Food and Drug Administration was recently launched and was not tested as part of Jokerst and Mantri’s study.)
“Ideally, these would all be built into the device. To have the end user fixing the measurement doesn’t make much sense,” Jokerst says.
He suggests that skin tone could be read from images obtained using a built-in CCD camera and that oxygen saturation measurements could be automatically adjusted using this information. Future work will evaluate the results of their proof-of-concept study in larger cohorts, against arterial blood gas measurements, and using a wider variety of imaging equipment.
Catherine Steffel is a science writer based in Madison, Wisconsin. Catherine was previously a PhD student contributor to Physics World.
from physicsworld.com 6/3/2022
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου