Low-dose radiation plus immunotherapy can eliminate metastatic cancer in mice
24 Aug 2021
Targeted radionuclide therapy (TRT) can increase the effectiveness of immunotherapy, helping to eradicate metastatic cancer in mice even when the radiation dose is too low to destroy the cancer outright. That’s the conclusion of a study by researchers at the University of Pittsburgh School of Medicine and the University of Wisconsin-Madison. Their findings, published in Science Translational Medicine, may lead to a new method for treating metastatic cancer, particularly for immunologically “cold” tumours that do not respond to immunotherapy.
Immune checkpoint inhibitors (ICIs) are immunotherapy drugs that block immune checkpoints, the part of the natural immune system that keeps immune responses from being too aggressive. Blocking these checkpoints allow immune cells to attack cancer cells more effectively. However, some patients have cancers characterized by immunologically cold tumours, which evade or suppress a patient’s immune response.
Preclinical studies have shown that external-beam radiotherapy (EBRT) targeting a single tumour can enhance response to ICIs. But even low-dose EBRT is not typically feasible for patients with metastatic cancers, due to the quantity of tumour sites, the presence of radiographically occult (invisible) tumours that cannot be readily targeted, and the toxicities that large-field or whole-body irradiation would cause. Ravi Patel and Zachary Morris. (Courtesy: UPMC/University of Wisconsin)
Ravi Patel and Zachary Morris. (Courtesy: UPMC/University of Wisconsin)
 Ravi Patel and Zachary Morris. (Courtesy: UPMC/University of Wisconsin)
Ravi Patel and Zachary Morris. (Courtesy: UPMC/University of Wisconsin)Lead author Ravi Patel and senior author Zachary Morris hypothesized that low-dose TRT might enhance a patient’s response to ICIs. TRT uses a cancer-targeting molecule to deliver a radionuclide to a tumour. As this radionuclide decays, it deposits radiation in the tumour microenvironment – providing a safe method to deliver radiation selectively to tumour sites. TRT is being developed for treatment of many types of cancer, however, no TRT has been tested to determine how it affects response to ICIs.
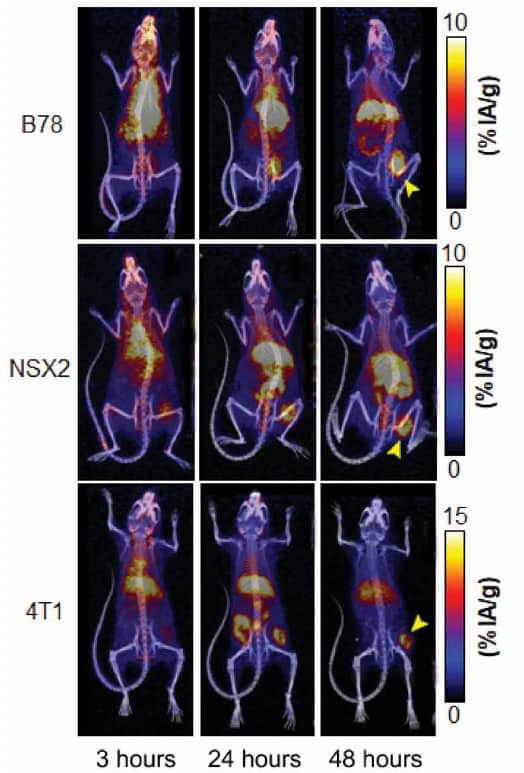
For this investigation, the researchers used NM600, a theranostic TRT that preferentially accumulates in most tumour types. NM600 can be used for both diagnostic imaging (86Y-NM600) or delivery of therapeutic radiation (90Y-NM600).
The researchers studied mice with B78 melanoma tumours, injecting the animals with 0, 25, 50 or 100 μCi of 90Y-NM600 (delivering 0, 1.25, 2.5 or 5.0 Gy to the tumour), either alone or combined with the ICI anti-CTLA-4 or dual ICI (anti-CTLA-4 plus anti-PD-L1). Mean tumour growth as a function of TRT dose (C4: anti-CTLA-4; VO: vehicle-only control). (Courtesy: Sci. Transl. Med. 13:eabb3631)
Mean tumour growth as a function of TRT dose (C4: anti-CTLA-4; VO: vehicle-only control). (Courtesy: Sci. Transl. Med. 13:eabb3631)
 Mean tumour growth as a function of TRT dose (C4: anti-CTLA-4; VO: vehicle-only control). (Courtesy: Sci. Transl. Med. 13:eabb3631)
Mean tumour growth as a function of TRT dose (C4: anti-CTLA-4; VO: vehicle-only control). (Courtesy: Sci. Transl. Med. 13:eabb3631)Mice receiving 50 or 100 μCi of 90Y-NM600 plus anti-CTLA-4 had significantly improved tumour response and increased survival compared with the group receiving either 90Y-NM600 or anti-CTLA-4 alone. Treatment with 90Y-NM600 plus dual ICI improved survival significantly compared with dual ICI alone.
“Only mice receiving combination TRT plus ICI treatment exhibited durable complete responses, and this represented about half of the group that received both therapies,” the researchers write. “All mice that achieved complete response exhibited immunologic memory against the tumour they had rejected and did not develop cancer again when they had the same type of melanoma tumour cells implanted 90 days later.”
The team also compared the therapeutic efficacy of 2.5 Gy of radiation delivered to a single tumour via targeted EBRT, whole-mouse EBRT or systemically delivered 90Y-NM600, either alone or in combination with anti-CTLA-4.
The whole-mouse EBRT was the least effective treatment, while anti-CTLA-4 plus low-dose targeted EBRT or 90Y-NM600 both increased tumour response. One advantage of radiation delivery via TRT over EBRT, the researchers note, is that TRT can treat all sites of metastatic disease, including those that are radiographically occult.
The mice experienced no visible toxicity from the combination of 90Y-NM600 and anti-CTLA-4, such as weight loss, lethargy or hunched posture. Histological analysis performed 35 days after TRT administration revealed no evidence of toxicity in the animals’ liver, spleen, bone marrow, small intestine or kidneys.
Proof-of-concept study
To examine the feasibility and safety of this approach in larger mammals, the researchers also treated two pet dogs with spontaneous metastatic cancer. The dogs received low-dose radiation to all tumour sites using 90Y-NM600, together with single-tumour-directed, moderate-dose EBRT.
“Because the range of radiation emitted from TRT agents is constant regardless of tumour context, these large animals more closely mimic the setting that will be encountered upon clinical translation of this combined modality approach in humans,” the team explain. The dogs tolerated this treatment combination well without toxic side effects.READ MORE

Further advantages of NM600, which was developed by co-authors Jamey Weichert and Reinier Hernandez, include its ability to semi-selectively deliver radionuclides to nearly any type of tumour, to cross the blood–brain barrier and to rapidly clear from blood. A Madison, WI-based start-up company, Archeus Technologies, is now completing studies needed to apply for approval from the US Food and Drug Administration to begin testing this agent in human clinical trials within the next one to two years.
In Patel’s lab, meanwhile, researchers are currently expanding upon this initial work by testing the concept with approved cancer therapies, such as 177Lu-PSMA and 177Lu-dotatate, with the goal of translating this treatment approach into the clinic. Patel notes that while combination low-dose TRT with ICI achieved high complete response or long-term cure rates, a proportion of tumours did eventually progress. As such, his lab is also investigating mechanisms of resistance to this therapy and strategies to overcome this resistance.
from physicsworld.com 1/9/2021
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου