Plastic scintillation detectors ready to shine as FLASH radiotherapy gathers momentum
28 Jan 2022 Sponsored by Medscint
Canadian technology start-up Medscint is working with customers to develop a new generation of real-time, small-field dosimetry solutions based on plastic scintillation detectors
Ultrahigh-dose-rate FLASH radiotherapy – whether using electron, proton or photon treatment beams – is shaping up as the “next big thing” in radiation oncology research. It’s easy to see why: a growing body of evidence – comprising preclinical experiments as well as the first small-scale clinical studies using electron and proton beams – demonstrates that radiation delivered at ultrahigh dose rates (roughly 40 Gy/s and above) can drastically reduce collateral damage and toxicity in normal healthy tissue while preserving anti-tumour activity.
Even so, it’s still early days and much work remains to be done before the at-scale clinical translation of FLASH radiotherapy becomes reality – not least the commercial development of affordable FLASH treatment machines as well as core enabling technologies such as FLASH treatment planning systems and robust dosimetry solutions for real-time beam monitoring. In the meantime, to fast-track commercial and clinical translation, medical physicists are redoubling their efforts to understand the fundamental radiobiology of the FLASH effect and, in turn, unlock research insights that will maximize the clinical impact of FLASH modalities for enhanced patient outcomes.
Online dosimetry
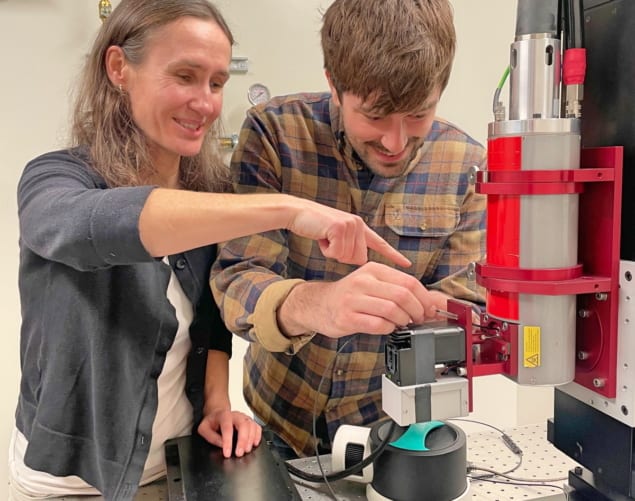
With this in mind, a team of scientists at the University of Victoria in British Columbia, Canada, has developed a cost-effective X-ray-tube-based system that exploits a customized beam shutter for in vitro ultrahigh-dose-rate irradiation (up to 118 Gy/s) of small samples with exposure times of less than 1 s (and latterly as short as 1 ms). Alongside the beam shutter and sample holder – which are designed and installed in close proximity to the X-ray tube window – one of the main building blocks of the benchtop system is a real-time, small-field dosimetry solution based on plastic scintillation detectors developed by Medscint, a specialist technology company in Quebec City.
“Plastic scintillation detectors are an ideal dosimeter for ultrahigh-dose-rate radiotherapy,” explains Magdalena Bazalova-Carter, lead physicist on the project and head of the X-ray Cancer Imaging and Therapy Experimental (XCITE) Lab at the University of Victoria. “By placing the scintillation detectors in close proximity of the beam shutter,” she adds, “we’ve been able to verify dose delivery and confirm that our system can accurately expose for short pulses down to 1 ms duration.”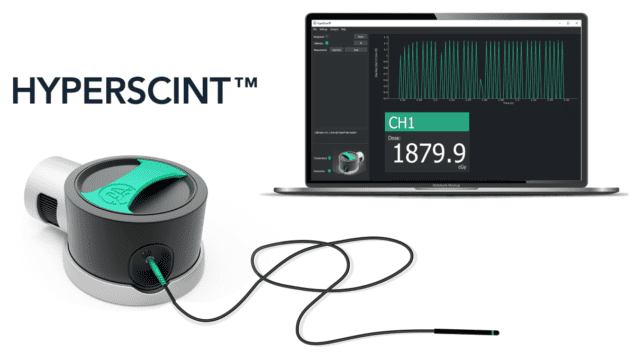 Scintillation dosimetry: Medscint’s initial product, the HYPERSCINT Research Platform, is targeted at R&D teams working on next-generation radiotherapy systems. (Courtesy: Medscint)
Scintillation dosimetry: Medscint’s initial product, the HYPERSCINT Research Platform, is targeted at R&D teams working on next-generation radiotherapy systems. (Courtesy: Medscint)
 Scintillation dosimetry: Medscint’s initial product, the HYPERSCINT Research Platform, is targeted at R&D teams working on next-generation radiotherapy systems. (Courtesy: Medscint)
Scintillation dosimetry: Medscint’s initial product, the HYPERSCINT Research Platform, is targeted at R&D teams working on next-generation radiotherapy systems. (Courtesy: Medscint)More broadly, plastic scintillators combine near-water-equivalence, nanosecond response times and high spatial resolution with MR-Linac compatibility and robustness against radiation damage.
Another advantage of the Medscint detectors is their compact footprint (0.5 mm long, 0.5 mm diameter), which makes them ideal for small-field and multipoint dosimetry. That’s a “must-have” for Bazalova-Carter and colleagues as their X-ray tube system is optimized for uniform dose delivery across samples no bigger than 6 mm in diameter.
In the lab, the XCITE team is currently putting the prototype X-ray tube system through its paces in a series of very-small-animal experiments, irradiating fruit fly larvae with ultrahigh dose rates and tracking comparative survival versus conventional irradiation schemes. “The early results are promising,” notes Alex Hart, a PhD student within the XCITE programme, “plus we’re now looking at the possibility of adding Medscint scintillation detectors to provide real-time, online readout of dose delivery.”
Put another way: it’s all about granularity. Inserting a small radiochromic film into the sample holder while irradiating the larvae provides the dose after the fact – i.e. if the dose is off for some reason, it’s not easy to figure out the root cause. “With a plastic scintillator in there,” Hart explains, “I could see that perhaps one of the exposures of a multipulse delivery didn’t happen at all or that it was shorter than expected.”
Beyond these proof-of-concept experiments, the next step for XCITE researchers is to deploy their X-ray tube system in the irradiation of normal and cancerous skin cells fabricated with 3D printing methods. Depending on the cell line, these so-called “multicellular cell spheroids” can be grown in a uniform fashion, such that their size can be controlled to within 5% – which, in turn, results in an interspheroid dose delivery difference of less than 1.1%. “Later this spring,” explains Hart, “we’ll use the X-ray tube system to investigate normal and cancer-cell spheroid response to ultrahigh dose rates and conventional irradiations – in each case, with and without gold nanoparticles as radiosensitizers.”
FLASH frontiers
Along a parallel line of enquiry, the XCITE team is also building a FLASH irradiation station on the ARIEL beamline at TRIUMF, the high-energy physics laboratory in Vancouver. To date, Bazalova-Carter, PhD student Nolan Esplen and colleagues have designed an electron-to-photon converter for the delivery of an ultrahigh dose-rate 10 MV photon beam on ARIEL’s existing medium-energy beam dump. Over the next three months, that cutting-edge capability will be evaluated in a series of experiments to investigate the FLASH effect on healthy lung tissue in mice.
Beam modelling suggests that the achieved dose rates at the irradiation site should be up to 200 Gy/s and above the FLASH effect dose-rate threshold of 40 Gy/s to depths of 10 cm. Here again, the R&D collaboration with Medscint will be pivotal. “We’ll use the Medscint plastic scintillators for in vivo dosimetry at TRIUMF, while evaluating scintillator response in the MV regime – something we haven’t done as yet,” explains Bazalova-Carter. “We’re also keen to work with the Medscint team to push the temporal resolution of the detectors further, down beyond the 1 ms exposure time into the microsecond regime.”
Looking further ahead, over the next 18–24 months, the XCITE R&D programme on spatially fractionated radiation therapy (SFRT) provides another opportunity for collaboration with Medscint’s development engineers. SFRT involves delivery of a single high dose fraction in a deliberately heterogeneous fashion – i.e. with high doses within the target volume as well as regions of underdosing – and shows great promise for the reduction of side-effects while maintaining efficacy for killing tumour cells. “We are developing custom hardware for SFRT beam delivery,” concludes Bazalova-Carter, “but we’re interested to see what we can achieve in partnership with Medscint on innovative SFRT dosimetry solutions.”
FROM PHYSICSWORLD.COM 30/1/2022
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου