Cardiac PET scans could predict the onset of neurodegenerative disease in at-risk individuals
03 Jan 2024
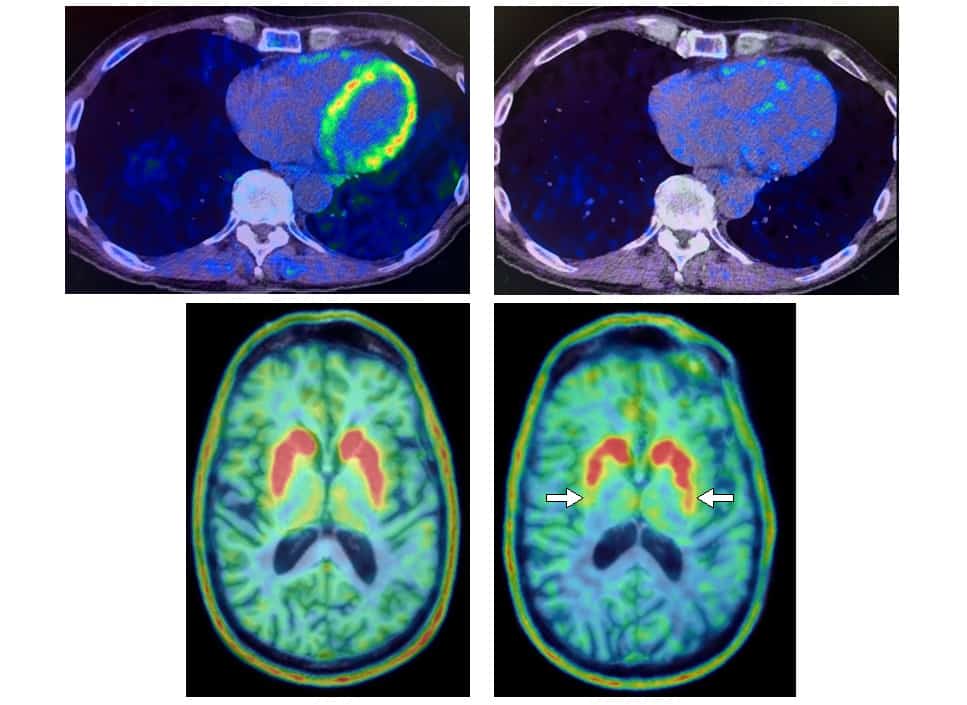
Early detection Heart and brain PET scans from a study participant who developed Parkinson’s disease support a “body first” progression. The top scans show low 18F-dopamine-derived radioactivity in the heart (right) and a normal 13N-ammonia PET scan (left), which preceded a loss of dopamine-producing neurons and symptom onset. (Courtesy: David S Goldstein lab/NINDS)
Researchers have been trying to answer questions about Parkinson’s disease and Lewy body dementia – including where these neurodegenerative diseases start – for decades.
“Where does Parkinson’s or dementia with Lewy bodies begin? You think, of course the brain. These are brain diseases,” says David Goldstein, a principal investigator at the National Institute of Neurological Disorders and Stroke.
But research by Goldstein and others has contributed to a “body first” hypothesis. That earlier work demonstrated, in part, that people with Lewy body diseases have depleted cardiac norepinephrine, which is normally released by nerves supplying the heart. (Norepinephrine is derived from dopamine, a neurotransmitter with low levels in the brains of people with Parkinson’s disease.)
The latest research by Goldstein and his team, now published in the Journal of Clinical Investigation, suggests that 18F-dopamine PET scans of the heart could be used to identify at-risk people who will go on to develop Parkinson’s disease or Lewy body dementia.
PDRisk Study
Based on their research from the late 1990s, which demonstrated that 18F-dopamine PET scans could separate three autonomic synuclein disorders (brain diseases characterized by abnormal deposits of the protein α-synuclein that form clumps called Lewy bodies), the researchers hypothesized that people who have multiple risk factors for Parkinson’s and who have a loss of sympathetic nerves in the heart will go on to develop symptomatic disease. They tested their hypothesis through the PDRisk Study, a prospective, observational research study that ran for nearly 15 years before it ended in 2023.
In the PDRisk Study, 34 participants at risk for Parkinson’s had cardiac 18F-dopamine PET scans every 18 months for up to 7.5 years, or until they were diagnosed with the disease. Participants had three or more Parkinson’s risk factors (family history of the disease, loss of sense of smell, dream enactment behaviour, and/or symptoms of orthostatic intolerance). Imaging protocols included 18F-dopamine PET and 13N-ammonia PET scans of the heart, plus 18F-DOPA scans of the brain (the 13N-ammonia scans ruled out diagnoses of other conditions that might contribute to loss of sympathetic nerves in the heart).
The researchers found that at-risk individuals with low 18F-dopamine-derived radioactivity in the heart were more likely to develop Parkinson’s or Lewy body dementia during follow-up, compared with individuals having the same risk factors but with normal radioactivity PET scans. Of the nine participants with low cardiac 18F-dopamine-derived radioactivity at their first PET scan, eight were later diagnosed with Parkinson’s or Lewy body dementia. Only one of 11 participants with normal initial radioactivity developed a central Lewy body disease.
‘Rolls Royce’ of cardiac sympathetic imaging
Once injected, 18F-dopamine is quickly taken up by sympathetic nerves and then stored in vesicles. Levels of “normal” and “low” 18F-dopamine-derived radioactivity in the PDRisk Study were determined from a 2011 Journal of Clinical Investigation paper that summarized 18F-dopamine radioactivity data from different relevant participant groups and were confirmed using three years of follow-up data from the PDRisk Study.
“The vesicular storage process is very energy-requiring. If you have a storage deficit – a ‘sick but not dead phenomenon’ where the nerves are there, but they’re sick – the slope of decline in radioactivity is much faster than usual,” explains Goldstein. “If there’s an energy crisis, or the vesicular uptake process is deficient, 18F-dopamine is shunted towards 18F-DOPAC, and radioactivity would come out. The slope of decline in radioactivity would be steep.”
Evidence of this was observed in the PDRisk Study, Goldstein says.READ MORE
“Most studies about treating Parkinson’s have been about trying to slow the neurodegenerative process…but they have started with people who are symptomatic. And that means you’re working at a severe disadvantage, because most of the neurodegeneration has already happened,” says Goldstein. “I’m not interested in treating or slowing the progression of symptomatic disease. I’m interested in preventing or delaying the onset of symptomatic disease. I think we have a way now to predict who, at least in people who have multiple risk factors, are going to develop a symptomatic central Lewy body disease during follow-up.”
Currently, 18F-dopamine PET scanning is only available at the National Institutes of Health (NIH) Clinical Center, where the study was performed.
“I do want to spread the word about 18F-dopamine PET scanning. It’s the Rolls Royce of cardiac sympathetic imaging. Other institutions in the United States don’t offer 18F-dopamine scans because insurance doesn’t cover it because it’s research. It’s research because other institutions don’t offer it. It’s a Catch-22 that I haven’t been able to solve yet,” Goldstein says.
Catherine Steffel is a science writer based in Madison, Wisconsin. Catherine was previously a PhD student contributor to Physics World.
FROM PHYSICSWORLD.COM 14/01/2024
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου