Light therapy fast-tracks healing of radiotherapy skin damage
15 Feb 2022 Tami Freeman

Brachytherapy is a cancer treatment in which a seed containing an ionizing radiation source is implanted directly within the tumour. The localized nature of brachytherapy enables delivery of high radiation doses to the target lesion while minimizing exposure of surrounding healthy tissues, reducing the risk of side effects. The treatment can, however, cause localized skin damage such as radiodermatitis and radionecrosis.
A research team headed up at University at Buffalo has investigated whether photobiomodulation (PBM) – a form of low-dose light therapy – could mitigate such skin damage. Motivated by reports on its efficacy for healing radiation damage and chronic wounds, the team demonstrated that PBM can speed tissue healing in mice with implanted iodine-125 (125I) brachytherapy seeds.
“To our knowledge, this is the first report on the successful use of photobiomodulation therapy for brachytherapy,” says senior author Praveen Arany in a press statement. “The results from this study support the progression to controlled human clinical studies to utilize this innovative therapy in managing the side effects from radiation cancer treatments.”
In vivo investigations
Arany and colleagues, also from the Nuclear and Energy Research Institute (IPEN) and the Federal University of Rio de Janeiro, subcutaneously implanted 125I brachytherapy seeds in 18 mice. They divided the animals into three groups, for treatment with: brachytherapy alone; brachytherapy plus PBM with red light; and brachytherapy plus PBM with near-infrared (NIR) light. Two further groups of mice received red or NIR light alone, and one group acted as untreated controls.
The team delivered PBM therapy using red (660 nm) or NIR (880 nm) LEDs with a 1 cm2 beam spot, an irradiance of 40 mW/cm2 and a fluence of 20 J/cm2. Treatments started on day zero and were repeated once per week over the site of the seed for 60 days.
In all mice, the first signs of skin radionecrosis appeared 21 days after seed insertion, when the total radiation dose reached roughly 8.5 × 104 Sv. Analysing digital images of the wounds revealed that PBM significantly reduced the incidence and severity of skin damage, particularly when using red light. Without PBM, wounds took an average of 61 days to heal. With NIR light, healing occurred within an average of 49 days, while red light therapy reduced the healing time further to an average of 42 days.
Radiation-induced tissue damage can lead to reduced blood perfusion and prolonged inflammation. To evaluate these parameters in the mice, the researchers performed laser Doppler flowmetry (to assess blood flow) and thermal imaging of the radiation-damaged skin every seven days. At 42 days post-seed implantation, when skin damage was maximal in the brachytherapy-alone group, the PBM-treated mice exhibited improved blood perfusion and significantly reduced inflammation.
The researchers also performed µPET-CT with the tracer 18F-FDG to assess tissue metabolism, which can be impacted by irradiation. At 42 days, they saw significant tracer uptake around the 125I seed in the brachytherapy-alone group. The NIR PBM-treated group demonstrated lower and less accentuated uptake around the seed, while the FDG signal was least prominent in the red PBM-treated group, indicating the lowest metabolic changes.
These observations correlate with the findings that brachytherapy side-effects such as inflammation and tissue damage are significantly attenuated by PBM therapy. The researchers also validated the changes via histological analysis, with one animal per group sacrificed at 42 days.
As PBM therapy becomes increasingly popular for use alongside brachytherapy, potential off-target effects on tumour cells could cause concern. The researchers note that evidence to date suggests that while PBM has a modulatory effect on normal cellular responses, it appears to have an inhibitory response on tumour cells. They emphasize, however, that these responses need to be investigated further.READ MORE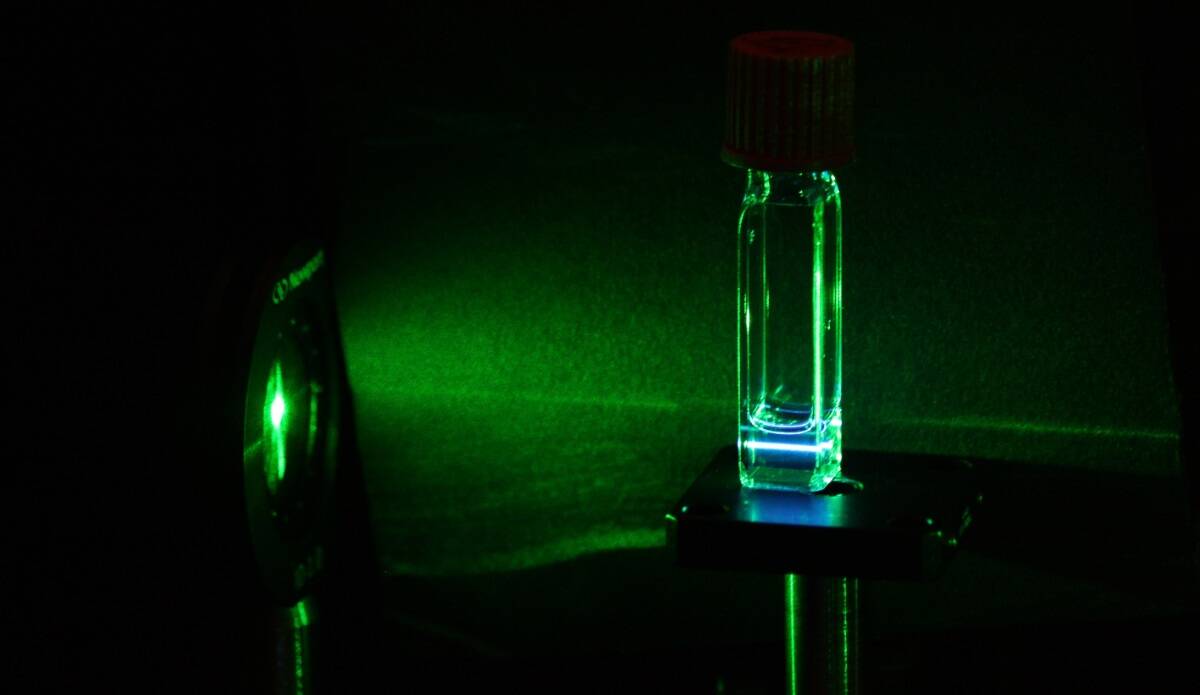
The team is currently evaluating the efficacy and molecular pathways of PBM therapy for managing skin radionecrosis in mice, mimicking the side effects of brachytherapy for prostate and ovarian cancer in humans. “For this, we had to produce equipment with specific optical properties, such as wavelength, power density and spot size, and we used LED-based equipment,” first author Rodrigo Mosca tells Physics World.
“In addition, we validated the LED-based devices against laser-based devices,” Mosca adds. “With this, we were able to drastically reduce the cost of PBM treatment, making it more affordable, with the same level of confidence and accuracy as laser equipment. For some treatments, there is still a difference, but in general, this is a great advance for PBM.”
The researchers report their findings in Photonics.
from physicsworld.com 24/2/2022
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου